Dr. Michael Chen had been practicing for 15 years when a seemingly routine lower back pain case changed his perspective forever. The patient, a 45-year-old construction worker, presented with familiar symptoms - localized pain, muscle tension, restricted movement. Based on clinical examination alone, it appeared to be a straightforward mechanical issue.
But something made Dr. Chen order imaging. The X-rays revealed what his hands couldn't detect: early-stage degenerative changes with concerning joint space narrowing that would significantly impact treatment planning. Without this objective data, he would have proceeded with standard adjustments that might have provided temporary relief but failed to address the underlying structural changes requiring a modified approach.
This case illustrates a fundamental principle in modern chiropractic care: clinical intuition and manual examination, while essential, must be supported by objective diagnostic information to deliver truly comprehensive patient care.
The Evolution of Evidence-Based Chiropractic Practice
Chiropractic care has evolved significantly from its early days of relying solely on palpation and clinical observation. Today's practitioners understand that optimal patient outcomes require a multi-faceted diagnostic approach that combines:
Clinical Assessment: Physical examination, orthopedic testing, and neurological evaluation provide crucial information about functional status and symptom presentation.
Patient History: Understanding mechanism of injury, symptom progression, and previous treatments offers context for current presentation.
Objective Imaging: Radiological studies reveal structural abnormalities, degenerative changes, and pathological conditions that may not be apparent through clinical examination alone.
When Clinical Examination Isn't Enough
Even the most experienced chiropractors encounter cases where clinical findings don't tell the complete story. Consider these scenarios:
The Hidden Fracture: A patient reports minor trauma with moderate pain. Clinical examination suggests muscle strain, but imaging reveals a hairline fracture requiring immediate modification of treatment approach and possible referral.
Degenerative Changes: Chronic pain patients may present with symptoms that seem disproportionate to clinical findings. Radiological evaluation can reveal advanced degenerative joint disease, spinal stenosis, or other structural changes that explain symptom severity and guide treatment planning.
Contraindications to Manipulation: Certain pathological conditions create absolute or relative contraindications to spinal manipulation. These conditions - including tumors, infections, severe osteoporosis, or vascular abnormalities - may not be detectable through clinical examination alone.
Red Flag Conditions: While rare, serious pathologies can present with common musculoskeletal symptoms. Imaging helps rule out conditions like metastatic disease, osteomyelitis, or cauda equina syndrome that require immediate medical intervention.
The Science Behind Objective Documentation
Research consistently demonstrates the value of imaging in chiropractic practice:
Diagnostic Accuracy: Studies show that combining clinical examination with appropriate imaging significantly improves diagnostic accuracy compared to clinical assessment alone.
Treatment Outcomes: Patients whose treatment plans are based on comprehensive diagnostic information, including imaging findings, demonstrate better long-term outcomes and higher satisfaction rates.
Risk Management: Objective documentation protects both patient safety and practitioner liability by ensuring appropriate care decisions based on complete diagnostic information.
Insurance and Legal Documentation: Third-party payers increasingly require objective findings to support treatment necessity and duration.
Understanding Imaging Modalities in Chiropractic Practice
Different imaging techniques provide unique diagnostic information:
Plain Film Radiography: Excellent for evaluating bone structure, joint alignment, degenerative changes, and ruling out fractures or gross pathology. Cost-effective and widely available.
CBCT (Cone Beam CT): Provides three-dimensional visualization of bony structures with lower radiation exposure than traditional CT. Particularly valuable for complex spinal anatomy and temporomandibular joint evaluation.
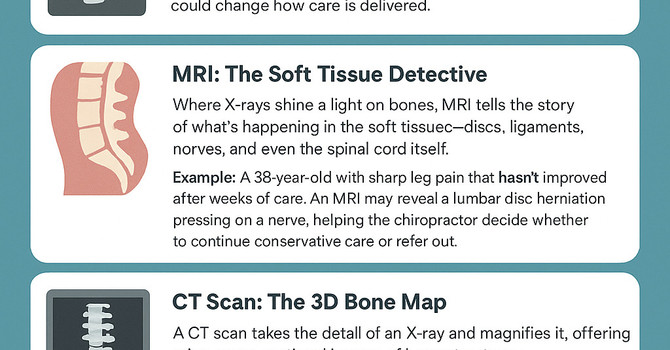
MRI: Superior soft tissue contrast makes MRI ideal for evaluating disc pathology, nerve compression, ligamentous injury, and ruling out serious pathology.
Functional Imaging: Dynamic studies can reveal instability patterns and movement abnormalities not apparent on static images.
Integrating Imaging into Clinical Decision-Making
Effective use of radiology requires understanding when imaging adds value to patient care:
Acute Trauma: Any significant trauma mechanism warrants imaging to rule out fracture or instability before manual treatment.
Neurological Symptoms: Radicular symptoms, progressive weakness, or bowel/bladder changes require imaging evaluation.
Treatment Failure: Patients who don't respond to appropriate conservative care within expected timeframes may have underlying pathology requiring imaging evaluation.
Chronic Conditions: Long-standing symptoms may indicate degenerative changes that influence treatment planning and prognosis.
The Role of Specialized Interpretation
While chiropractors are trained in radiological interpretation, complex cases benefit from specialized expertise. Diplomates of the American Chiropractic Board of Radiology (DACBRs) provide:
Advanced Training: Extensive post-graduate education in musculoskeletal imaging interpretation Specialized Focus: Expertise specifically in conditions commonly seen in chiropractic practice Objective Analysis: Independent interpretation free from treatment bias Comprehensive Reporting: Detailed findings with clinical correlations and recommendations
Building an Objective Care Framework
Implementing objective care principles requires systematic approach:
- Establish Clear Imaging Guidelines: Develop protocols for when imaging is indicated based on clinical presentation
- Choose Appropriate Modalities: Select imaging techniques that provide necessary diagnostic information
- Seek Expert Interpretation: Utilize specialized radiology expertise for complex cases
- Integrate Findings: Combine imaging results with clinical assessment for comprehensive treatment planning
- Document Thoroughly: Maintain detailed records supporting clinical decision-making
The Future of Objective Chiropractic Care
As healthcare continues to evolve toward evidence-based practice, chiropractors who embrace objective diagnostic approaches will be better positioned to:
- Deliver superior patient outcomes
- Demonstrate treatment necessity and effectiveness
- Collaborate effectively with other healthcare providers
- Meet evolving insurance and regulatory requirements
- Build patient trust through transparent, scientific care
Conclusion
The integration of appropriate imaging into chiropractic practice isn't about replacing clinical skills - it's about enhancing them. When clinical expertise combines with objective diagnostic information, chiropractors can deliver the comprehensive, evidence-based care that today's patients deserve and expect.
Every patient presents a unique diagnostic puzzle. Clinical examination provides crucial pieces, but imaging often reveals the complete picture necessary for optimal care decisions. By embracing objective diagnostic approaches, chiropractors honor both the art and science of their profession.